North West London Fellowship Programme
Applications open for the NWL Fellowship 2025/2026
Across North West London we have re-launched the Fellowship Programme and opened it not just to GPs and nurses that are new to practice, but to clinicians at different stages in their career and to other multi-professional roles within general practice. The new fellows will be working on projects in areas that support and meet local borough needs and North West London priority areas.
Eligibility criteria:
- The Fellow is working in a salaried role within General Practice for at least 16 hours per week for the duration of the fellowship.
- There is now no criterial for how long they have worked within General Practice and do not need to be new to practice.
- Have not undertaken a fellowship in the last 3 years (SPIN, Mid-Career, PG Cert etc)
Fellowship funding will cover 1 session a week for 12 months. Rates provided are inclusive of session rate and oncosts and paid to employers:
- GPs – £12,000
- Nurses and Multi-professionals- £6,000
There are limited spaces across all 8 boroughs so applicants will go through a shortlisting and interview process. Below are the offers from each local borough along with the application form to apply.
The application deadline has now passed.
If you have any questions, please contact your local borough or email [email protected].
APPLICATIONS NOW CLOSED
Brent Training Hub have proposed two fellowship offers, see below for more information.
Proposal for Health Equity Fellowship
Requirements: GP, no previous experience required, but enthusiasm and self-direction and a keen interest in health equity is essential.
Proposed fellowship project
The fellow will undertake a strategic leadership role focused on reducing health inequalities in Brent, aligned with national priorities and local needs. The project will be embedded within the development of Integrated Neighbourhood Teams (INTs) and will consist of:
Induction phase:
- Understanding and working:
- Local People
- Local Data
- Local Services
- Principles of designing and implementing efficient, productive and sustainable services using QSIR, PDSA or similar
Project phase:
- Support fledgling INTs to identify and establish local health inequality priorities.
- Facilitate the integration of Brent Health Matters (BHM) into INT structures to deliver on these priorities.
- Address inequities affecting both adults and children/young people, ensuring a “cradle-to-grave” approach.
- Embed community health workers within local neighbourhoods, working proactively with entire households. This will draw on elements of the Brasilian Family Health Strategy model, enabling a population-based, preventative approach.
The fellow will be given the opportunity to develop their leadership skills and shape the role.
The fellow will report to:
- Brent Health Inequalities Clinical Lead
- Brent Health Matters Programme Director
Both will provide general oversight, supervision, and mentorship throughout the fellowship.
What are the measurable outcomes would you expect from the fellowship.
- Integrated Neighbourhood Teams (NWL KPI): Successful embedding of health inequality priorities into INT strategic plans.
- Development and agreement of measurable local health inequality outcome indicators with individual INTs.
- Demonstrated improvement in health inequality outcomes within at least two local INT footprints.
- Number of households supported by community workers and progress against agreed health inequality outcome measures.
Proposal for GP Fellowship in Children and Young People’s Mental Health Integration (Brent)
We propose recruiting one GP fellow for a 12-month fellowship, no previous experience required, but enthusiasm and self-direction and a keen interest in children and young people’s mental health is essential.
Project focus
This fellowship will directly address Brent’s urgent need to strengthen early intervention and integration for children and young people’s mental health. Brent faces the greatest pressures across North West London, with Specialist CAMHS receiving 30 new referrals every day and holding the highest caseloads in the sector. As of July 2025, 3,300 children and young people were open to CAMHS, including 870 on the neurodevelopmental waiting list with an average wait of 30 months. Brent alone accounts for 45% of all CNWL CAMHS referrals (WSIC, June 2025), and in 2024/25, 40% of all A&E mental health presentations for children and young people across the eight NWL boroughs came from Brent. These figures highlight both overwhelming demand and a lack of early intervention, with many CYP only accessing support once they reach crisis.
After a period of upskilling and training alongside our CAMHS colleagues and other CYP MH colleagues in Brent (eg at VCSE organisations, early intervention services and the MHSTs) The GP fellow will play a pivotal role in addressing these challenges by:
- Providing mental health connection and support to all the Brent child Health Hubs – helping to embed CYP mental health expertise in all Brent CHH MDT meetings both by attending these hubs as a CYP MH representative (after a period of training and upskilling) and by ensuring that wider MDT colleagues from CYP MH services are encouraged to attend, ensuring early intervention is built into case discussions and care planning at neighbourhood level. They will play a key role in liaising with CAMHS and also publicising the other alternative support services that are available in the borough.
- Building primary care capability – delivering training, education sessions, and masterclasses for Brent GPs and practice staff to improve confidence in managing CYP mental health. They will work on further refining and promoting the borough’s existing signposting materials, and working to embed them into the JOY/EMIS systems so that we can reduce inappropriate referrals, and strengthen the quality of early support.
- Supporting triage and multi-agency coordination – contributing to the single point of access triage processes and MDT referral pathways, working alongside CAMHS, schools, social care, and VCSE partners to ensure a “no wrong door” approach and timely allocation of children and families to the most appropriate support.
A single point of access for CYP Mental health concerns in Brent is being developed and this is a key moment for a fellow to benefit from this service development and leadership opportunity, gain valuable CYP mental health skills and contribute essential primary care perspective to the service.
By working across these three domains, the fellow will strengthen integration, improve early access to care, and help reduce Brent’s reliance on overstretched specialist and emergency services.
Reporting and oversight
The fellow will require clinical supervision from both pediatrics (via the already established links with the child health hubs) and CAMHS. General oversight will be provided by the Brent ICP clinical lead for children’s service who is part of the strategic group for the CYP MH transformation. The local training hub will provide educational supervision.
Expected measurable outcomes (KPIs)
We propose the following KPIs, aligned to local needs and NWL priority areas:
- Integration (NWL priority: Integrated Neighbourhood Teams) – Attend and contribute to at least 75% of Child Health Hub MDTs, with evidence of improved multi-agency coordination (measured through professional feedback and case tracking).
- Access – Increase the proportion of CYP seen in early intervention settings (e.g. schools, hubs, GP clinics)
- Education – Deliver education and training sessions for at least 20 GPs and primary care staff, with 80% reporting improved confidence in managing CYP mental health presentations.
- System outcomes – Demonstrate a reduction in inappropriate CAMHS referrals from participating PCNs
If you are interested in applying to either of the fellowships please complete the below application form and upload a personal statement demonstrating why you are a suitable candidate.
Important Note for all Ealing Fellowship roles: Preference will be given to those who can do the session on a Wednesday or Thursday as these are the days that most of the meetings concerning these workstreams take place.
Project area: Integrated Neighbourhood Teams
Role requirement: Any clinician with suitable expertise
Reporting and Oversight: Head of Programmes and Ealing Training Hub
The fellow will provide clinical leadership for the development and implementation of increasing physical activity initiatives across the 8 Integrated Neighbourhood Teams (INTs). The work will involve:
- Identifying priority clinical cohorts who would benefit most from increasing physical activity interventions (e.g. people with long-term conditions such as diabetes, COPD, cardiovascular disease, frailty, or mental health needs).
- Using population health data and local intelligence to target cohorts with the highest unmet need or health inequalities.
- Leading on the borough-wide increasing physical activity agenda and collaborating with Sport England, London Sport, the Chief Leisure Officer, and other relevant professionals.
- Establishing borough-level and INT-level plans that embed increasing physical activity into clinical pathways and preventative care models.
- Identifying and supporting INT-level increasing physical activity representatives to champion this agenda across all 8 INTs.
- Applying the “Four Ways Forward” (and other relevant frameworks) to co-design and test clinically relevant initiatives (e.g. exercise referral schemes, falls prevention, cardiac rehabilitation, social prescribing).
- Empower clinicians and health and care professionals with the skills and confidence to discuss and promote physical activity, integrating it into key clinical pathways, aligning it with Core20PLUS5 for adults, children and young people.
- Working closely with INT Clinical and Managerial Leads to ensure increasing physical activity is promoted within primary care and linked into INT multidisciplinary working.
- Representing Ealing INTs at local and regional increasing physical activity work groups, and networks, ensuring local clinical priorities and learning are shared and aligned with regional strategies.
- Identifying and monitoring VCFSE sector programmes that deliver increasing physical activity, ensuring crucial partners are connected into the appropriate INTs and linked to relevant patient cohorts.
- Identifying funding opportunities (local, regional, national) to support and expand clinically targeted increasing physical activity initiatives.
KPIs and Outputs:
- KPI: At least 2 priority clinical cohorts identified in each INT across the borough (e.g. diabetes, COPD, frailty).
Output: A borough-wide report with INT-level breakdown showing target cohorts, prevalence, and inequality mapping. - KPI: Increasing physical activity plan developed and adopted in all 8 INTs.
Output: Each INT has a written action plan embedding increasing physical activity into at least one long-term condition pathway. - KPI: A minimum of 1 clinically relevant increasing physical activity initiative tested in each INT (e.g. falls prevention in frailty, activity coaching in mental health, community walking groups for COPD).
Output: Project briefs and evaluation reports for each initiative, including baseline and follow-up participation data. - KPI: At least 2 funding bids submitted or new funding streams secured for local increasing physical activity initiatives.
Output: Funding applications and confirmed grants/contracts to scale successful interventions.
Project Area: Access
Role requirement: Any clinician with suitable expertise
Reporting and Oversight: Medical Director and Ealing Training Hub
Measurable Outcomes:
- Review of GPAD data across PCN for practices and enhanced access hub and benchmarked against other comparable practices and PCNs
- Description of access models in place across PCN e.g total triage, online consultations and use of IT/AI platforms to help manage demand with a review
- Review of extended access hubs with a view to creating a business case and project plan for how vaccinations, smears and other enhanced services could be delivered via the enhanced access hubs
- Recruitment of 2- 4 patients per practice as a focus group for 3 meetings to be held during the year at start middle and end of project
- 1- 2 interventions trialed to improve access
- Project written up as case study
Project Area: Enhanced Services
Role requirement: Any clinician with suitable expertise
Reporting and Oversight: Assistant Director and Ealing Training Hub
Measurable outcomes:
- Identify one enhanced service that is not well taken up within PCN for example warfarin monitoring or IUCDs
- Map requirements of specification, numbers of potential patients and skills gap
- Work with training hub to identify training and mentors (for IUCD training) and look at how the work could be rotated across practices with associated referral pathways and safety netting
- Write up proposal for how service could be better delivered within the PCN
Project Area: Quality
Role requirement: Any clinician with suitable expertise
Reporting and Oversight: Medical Director and Ealing Training Hub
Measurable Outcomes:
- Identify an area of quality within PCN you would like to work on. Suggested topics: reducing vaccine hesitancy, creating a workforce strategy, digital inclusion
- Baseline data survey
- Project proposal to include 3 – 5 interventions to improve data
- Test interventions and write up as a case study
If you are interested in applying please download and complete the attached project proposal template and upload it to the application form below.
Please contact [email protected] for information relating to fellowships in Hammersmith and Fulham.
APPLICATIONS NOW CLOSED
We will be asking Fellows to work with our local Training Hub and Clinical Directors to create projects around the following borough priorities:
- Metabolic Health
- Complex Care
- Access
Role requirement: Ideally 1 GP and 2 AARSs clinicians, however others are welcome to apply
Reporting and Oversight: Depending on the project, a supervisor will be appointed. Fellows will report to Harrow Training Hub and the TH will have oversight.
Measurable Outcomes:
- Defining the relevant target population within a PCN/INT/borough
- A measurable improvement in the chosen area of work based on WISC data.
- Improved education and knowledge on the area for both staff in primary care and patients
- Introducing a change that can be continued into the future
If you are interested in applying please download and complete the attached project proposal template and upload it to the application form below.
Requirements: GPs would be preferred
Project Area: We would like ideas for Quality improvement projects that support vulnerable people and align with the Core20plus5
Reporting and oversight would depend on the project itself
We are looking for KPIs that will reduce inequality and increase positive health outcomes. Please include outcomes and KPIs in the project proposal.
If you are interested in applying please download and complete the attached project proposal template and upload it to the application form below.
Hounslow is proposing to recruit four nursing fellows to work across the five Primary Care Networks (PCNs) in the borough. This proposal responds to a clear local need for enhanced
nursing leadership and workforce development in primary care.
Proposed Fellowship Project
The fellowship will focus on re-establishing nursing leadership and education within primary care settings. We have observed a decline in nursing engagement with professional development and the implementation of enhanced services. Additionally, recruitment and retention of primary care nurses remain significant challenges.
The fellows will:
- Support existing primary care nurses through mentorship, education, and leadership development.
- Promotion of existing courses and development opportunities to our primary care nurse workforce, driving the quality of patient care.
- Work collaboratively with the PCN clinical directors to identify current local nursing issues and also how our nursing workforce can support with the delivery of local enhanced services and also improving access to services.
- Be a primary care nursing ‘voice’ on the PCN clinical meetings and also represent primary care nursing in the PCN INT projects.
- Promote career progression pathways and improve visibility of nursing roles in primary care.
Reporting an Oversight:
Each fellow will be:
- Attached to one or two PCNs, with day-to-day support from the PCN Clinical Director and PCN manager.
- Supported by Head of PCN Strategy and Development, who is herself a Nurse Leader; to provide strategic oversight and coordinate cross-PCN collaboration.
- Supported by the Hounslow Training Hub (both the Training Hub Lead and GP Educator),which will facilitate educational opportunities and monitor progress.
Measurable outcomes and KPIs:
We propose the following Key Performance Indicators (KPIs) to evaluate the impact of the fellowship:
- Increase in nursing engagement with CPD and local education initiatives (e.g., number of nurses attending borough-wide training sessions).
- Establishment of a borough-wide nursing leadership forum to promote shared learning and collaboration.
- Improved retention rates of primary care nurses across Hounslow PCNs.
- Primary Care Nurse input into the PCN INT projects; these projects are currently agreed at a PCN level and lacking primary care nurse input.
If you are interested in applying to either of the fellowships please complete the below application form and upload a personal statement demonstrating why you are a suitable candidate.
APPLICATIONS NOW CLOSED
Neighbourhood Health
Neighbourhoods are central to both national and local strategies aimed at improving the health and wellbeing of communities. This policy marks a significant shift in how services are delivered, with a greater emphasis on collaboration, local leadership, and place-based care. West London Fed is a key partner in the Bi-Borough Placed Based Partnership. The Partnership was successful in its application as a Wave One site in the National Neighbourhood Health Implementation Programme (NNHIP) which commences this Autumn. This is a large scale change programme that builds on the existing knowledge and experience to support places deliver care differently, generate the necessary changes in culture and integrated working and is a real opportunity to move things forward.
At the heart of this approach is the recognition that those closest to communities—particularly primary care—are well-positioned to lead innovative, locally tailored projects that respond directly to the unique needs of their neighbourhoods.
We are at the early stages of developing this strategy, and a “test and learn” approach will be essential. By supporting newly appointed Fellows to design and implement local health initiatives, we aim to identify what works well, share learning, and refine our approach as we go. This not only empowers the next generation of healthcare leaders but ensures that neighbourhood health evolves in a way that is responsive, evidence-informed, and rooted in local experience.
Overview of the Fellowship
This Fellowship aims to support clinical leadership in strengthening neighbourhood working, and addressing quality and equity across West London. A key focus will be on tackling health inequalities by identifying and addressing gaps in access, outcomes, and service provision for underserved populations.
Fellows will gain hands-on experience in clinical leadership and strategic planning, contributing directly to the transformation of neighbourhood models of care. They will play a key role in promoting health equity by addressing disparities and improving outcomes for underserved populations. Mentorship from experienced leads will support their development, while opportunities to collaborate with peers, neighbourhood teams, and system leaders across West London will enhance their professional network and influence.
There are 2 roles on offer. At least one will be a GP. The role is open to multi-professionals and GPs who will work closely with our Neighbourhood Leads in ensuring SMART goals are set to meet clear objectives. This is an exciting time to sign up as a Fellow and make a meaningful difference in neighbourhood ways of working.
The Fellows will also work closely with Clinical Directors (CDs), Education Leads, and Training Hub Lead taking a population health approach to identify disparities, develop targeted interventions, and implement sustainable improvements that promote equity.
Area of focus
- Neighbourhood Working: Strengthen collaboration across practices and local services to ensure coordinated care and equitable access. The project work should:
- reduce inequalities
- target and align with prevention priorities
- improve integrated neighbourhood working
- employ population health management principles
- We aim to build on the National Neighbourhood Health Implementation Programme (NNHIP), using a population health approach to bring our neighbourhoods together in preparation for improving the prevention and management of people with long term conditions, addressing neighbourhood inequalities and improving health outcomes across our local population.
Support Structure
Fellows will have a range of support from Federation colleagues including:
- Education Leads
- Neighbourhood teams
- Clinical Directors
- Training Hub Lead
- Data and analytical support
- Federation Strategy and Neighbourhood directorate
Role Requirements
Open to General Practitioners and multi-professionals working in the West London PCNs who are employed in a salaried role within General Practice for at least 16 hours per week. Able to commit for 12 month duration of the Fellowship.
Project Structure
- Use quantitative and qualitative data to identify areas of inequality and improvement.
- Assist PCNs in diagnosing issues such as staffing gaps, training needs, or service delivery barriers.
- Develop a structured work plan with measurable KPIs.
- Document the project as a case study for wider dissemination.
Expected Outputs
Outputs of the work undertaken by Fellows will be mutually agreed between the Fellow, PCN, and Training Hub. Examples include:
- Engagement with priority populations and measurable improvements in health outcomes.
- Increased uptake of services and prevention in underserved areas.
- Reduction in service variation across practices.
- Improved access or quality metrics for deprived cohorts.
Key deliverables :
- Baseline and follow-up data analysis.
- Written project proposal and implementation plan.
- Final report with recommendations, including impact on inequalities.
- Feedback and updates to West London Fed Board and sub-committees
Application Process
- Download and complete the Fellowship project proposal template below
- Fill the application form and submit the project template and a personal statement on this link.
- Deadline for application submission is midnight 23rd November 2025
- Upload the completed proposal to the application form provided.
- Interview of successful applicants w/c -1st / 8th December
APPLICATIONS NOW CLOSED
What does a Central London Training Hub Fellowship look like?
Exciting opportunities to all clinicians to Lead on key projects across the Borough, build a portfolio career where you can develop your own interest, make a difference to the local community and are paid to do so. Depending on your project, you will have a clinical and/or non-clinical educator either in HCL/NWL to support you on your journey.
The Central Training Hub is offering fellows the chance to lead on transformative projects that will shape the future of healthcare delivery.
Current Project Opportunities:
- Remote Hypertension Monitoring Rollout – Supporting patients to better manage blood pressure with digital solutions.
- RPA Bots Rollout – Harnessing Robotic Process Automation to streamline clinical and administrative workflows.
- Immunisations and screening – Tackling low uptake by addressing coding issues, patient mobility, and registrations
Opportunities include bespoke family meetings— fellows working alongside Public Health colleagues to engage families and boost vaccination confidence - Health inequalities - Working with our Health equity lead with a view to increasing chronic disease prevalence amongst other things
- Octopus – supervision and leadership of ARRS roles
Measurable Outcomes:
Will be clear and specific results that can be tracked with evidence — for example, setting targets such as the percentage of staff passing a post-training assessment, or the proportion of patients showing improvement within a set timeframe.
Why Join?
- Gain leadership and project management experience
- Collaborate with multi-disciplinary teams
- Drive innovation at scale
- Make a measurable difference in patient outcome
- Avail of mentoring support
If you are interested in applying please download and complete the attached project proposal template and upload it to the application form below.
Applications are currently closed but if you are interested in undertaking a fellowship please complete the form below and we will be in touch if new fellowship opportunities become available.
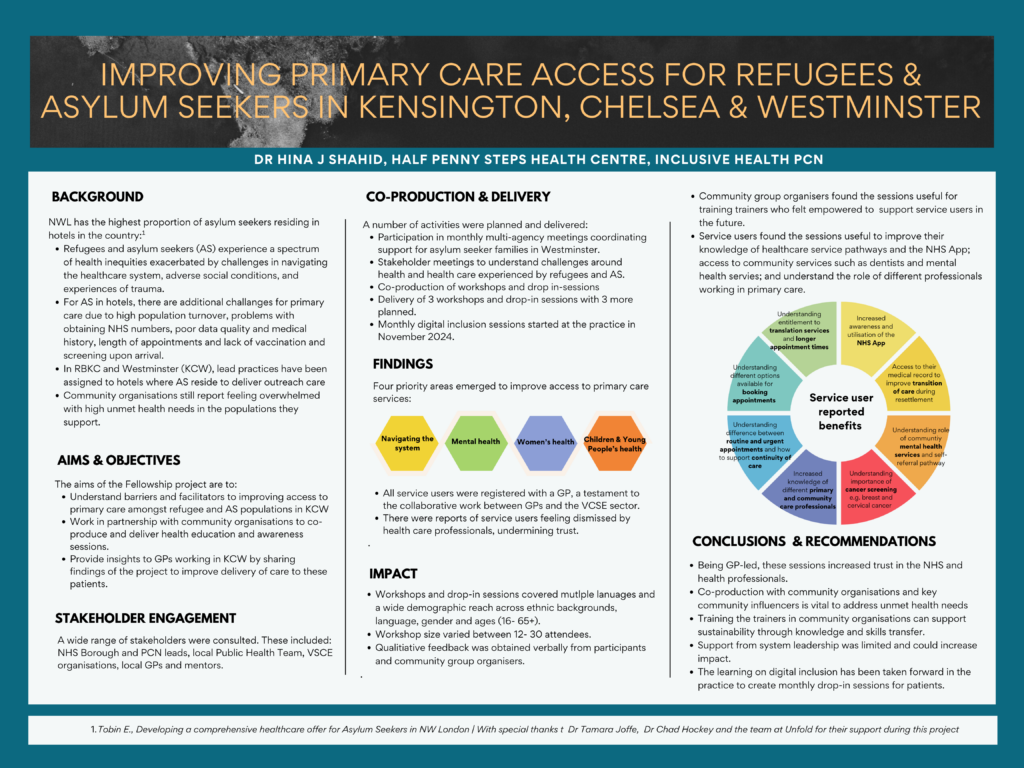
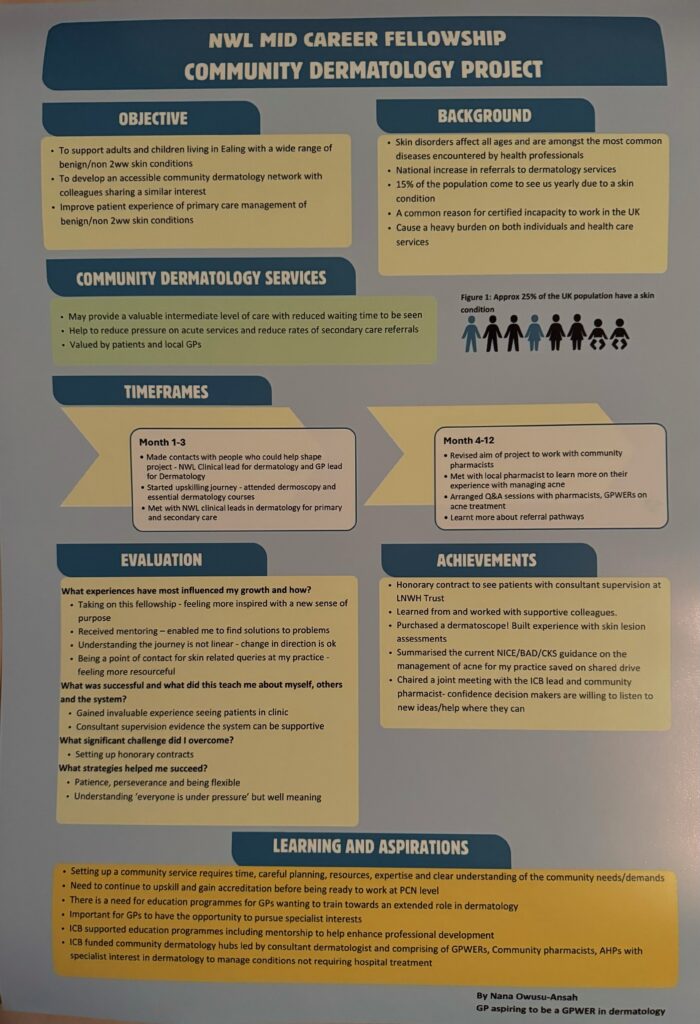
Latest news: GP Mid Career Fellowship Programme 2023/2024
In October 2023, we launched a GP mid-career Fellowship. The vision for this was to allow busy GPs some time and space to work on a project that they were passionate about and felt would make a difference to the communities they worked in. We hoped it would help to prevent burn out and help with retention of GPs within North West London.
On Friday 29th November 2024, we held a Showcase Event for the NWL Mid-Career GP Fellows, who completed their one-year Fellowship in October. This gave us the opportunity to come together and share experiences and to celebrate the work that has been done. These projects have created a huge positive impact to our local communities and rejuvenated GP’s, some of whom were previously on the brink of burnout.
The hard work and dedication to these projects was highlighted by the GPs in their presentations and this led to thought provoking conversations on how to better the health of the NWL population, especially those with health inequalities.
A huge well done to all of the Mid-Career GP Fellows!